Since returning to Chicago in the early aughts, I’ve been fortunate to find excellent doctors. Unfortunately, I’ve had to change doctors periodically because of the turnover in primary care and women’s health practitioners. Gynecologists and primary care physicians seem to burn out fairly regularly. The OB/GYN specialty has been particularly stressed, as economic pressures in healthcare systems have shifted routine or uncomplicated cases to certified nurse midwives, nurse practitioners, and physician’s assistants. That means that OB/GYN physicians are treating the trickiest and most dangerous conditions, e.g., high-risk pregnancies or patients with complicated co-morbidities. These doctors make life-and-death decisions every day. And the pressures on women’s health doctors are about to surge. When Roe v. Wade is canceled by the Supreme Court next month and women’s healthcare decisions are handed to state legislators, our revered doctors could be threatened with—not only lawsuits—but prison time.
My relationship with my gynecologist (who is the last person standing from the original three doctors in the group practice) is lighthearted and easy. I look forward to seeing her once a year and I follow her advice always. So I was thinking about all the crap that is about to fall on her shoulders when SCOTUS opens the gates to a mob of medically ignorant and ideological politicians with the power to write their preferences into law.
When Alito’s draft opinion in Dobbs v. Jackson was revealed, the American College of Obstetricians and Gynecologists (ACOG) released a statement
in defense of comprehensive reproductive medical care and against legislative interference in the patient–physician relationship. . . . As a new legal framework for abortion access unfolds, unexpected challenges continue to emerge regarding clinical, practice management, and logistical challenges. (Emphasis mine-m.o.)
On average, it takes 12 years of higher education to become a gynecologist. The educational requirements for a legislator are nil. What’s really infuriating is to witness a person with not even a basic understanding of human biology seek the power to make medical decisions for half the population. Remember Tea Party Republican, Todd Akin, of Missouri? During his Sentate campaign in 2012, a local TV reporter asked him why his anti-abortion position made no exception for rape. Akin responded,
It seems to me . . . that’s really rare. If it’s a legitimate rape, the female body has ways to try to shut that whole thing down.
The people making laws that restrict women’s bodily autonomy act on misinformation and prejudice. They are poised to make the practice of medicine a complete minefield. And if a doctor steps on one of the many hidden mines, she detonates her career. Or worse.
So, think about it. If you were a third year medical student applying for residencies and comparing different specialties . . . would obstetrics and gynecology be high on your list? Consider: on average, students graduate from medical school about $216,000 in debt. Orthopedic surgeons make about $200,000 more than OB/GYN doctors annually but their average cost of malpractice insurance in Illinois is $73,760 compared to OB/GYN malpractice insurance of $112,150. On top of the financial disincentive, in certain states you may face the possibility of arrest if an investigator decides that your treatment of a patient was unlawful. I wonder if any currently practicing obstetrician or gynecologist would advise a young person to go into their field?
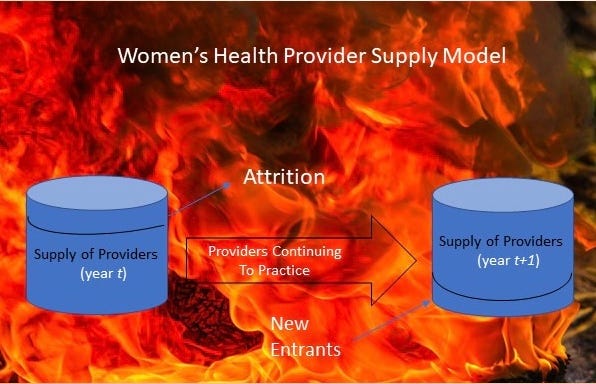
Social scientists in the Dept. of Health and Human Services periodically assess the workforce requirements in the health care field. They look across the country to determine where the need exists for different types of healthcare. In their 2018 report on women’s health, they examined where OB/GYN professionals were located and where they were needed. The analysts, using the supply-demand model pictured above, considered the effects of attrition (e.g., losing doctors because of retirements or other reasons) together with estimates of the numbers of new doctors entering the field. Then they project whether different areas of the country will have sufficient numbers of doctors in the future or whether they will have a deficit.
These are the projections for 2030, based on 2018 data:
By 2030, the Northeast is still projected to have an adequate number of OB-GYNs, while the other regions have deficits . . . . The supply adequacy at the state level will continue to show a large variation, ranging from less than 70.0% (New Mexico, Nevada, Utah, Oklahoma, Arkansas, and Iowa) to greater than 110% (Maryland, Connecticut, New York, Vermont, and Rhode Island), while the District of Columbia will again likely have an outlying level of supply adequacy (157.1%).
Exhibit 4 of the report shows that only the Northeast* will have an adequate number of OB/GYN doctors by 2030. The Midwest** will be short 500 doctors (95% supply adequacy), the South*** will lack 2,270 doctors (88.7% supply adequacy). The West**** will experience the highest deficit of OB/GYNs. They will lack 20% of the 13,690 doctors they need.
Here’s the kicker: the projection for 2030 was based on a “status quo scenario.” By the end of this summer (2022!), the current status quo will seem like a sweet dream of days gone by. Things will get a lot worse.
Keep scrolling down (below Notes) to reach the comments, share, and like buttons.
Notes:
*Northeast (CT, ME, MA, NH, NJ, NY, PA, RI, VT)
**Midwest (IL, IN, IA, KS, MI, MN, MO, NE, ND, OH,SD, WI)
***South (AL, AK, DE, DC, FL, GA, KY, LA, MD, MS, NC, OK, SC, TN, TX, VA, WV)
****West (AK, AZ, CA, CO, HI, ID, MT, NV, NM, WA, WY)
ACOG, A Message to the ACOG community regarding the future of abortion care.
John Eligon and Michael Schwirtz, Todd Akin provokes ire with “legitimate rape” comment.
Gallagher Healthcare, Illinois Medical Malpractice Insurance.
Clint Proctor, Is an OB/GYN salary worth the student loan debt?
US Departent of Health and Human Services, Projections of Supply and Demand for Women’s Health Service Providers, 2018-2030.
Yang Y, Li J, Wu X, et al. Factors influencing subspecialty choice among medical students: a systematic review and meta-analysis. BMJ Open 2019;9:e022097. doi: 10.1136/bmjopen-2018-022097.



Great article and I totally agree. In addition, sadly women of color often experience very different medical care in general.
Thank for an excellent article, which I will share to Fb. Every woman can relate to an access to Ob/Gyn care.